Health & Fitness
Most Women Will Experience Vaginal Dryness in Their Lifetime. So Why is the Topic Still Taboo?
It’s time to break the silence around this extremely common and easy-to-treat condition with Canadian experts and their simple solutions.
by : Joanie Pietracupa- May 9th, 2024

Photography:, GALLERY STOCK
When 52-year-old Emilie* started noticing vaginal-dryness symptoms for the first time eight or nine years ago, she thought they would pass. “I figured I was too young for that,” she says. “But when mere discomfort during sex turned into intense pain and sometimes bleeding, I decided to get in touch with my GP. It was one of the best decisions I’ve ever made. Although I felt totally awkward broaching the subject with my doctor—or anyone, really—I got the right treatment and the problem was solved.”
According to Dr. Lindsay Shirreff, an obstetrician and gynecologist at Mount Sinai Hospital in Toronto, vaginal dryness can be a symptom associated with genitourinary syndrome of menopause (GSM). “GSM refers to the collection of physical changes and symptoms involving the vulva, vagina, lower urinary tract and pelvic floor muscles,” explains Shirreff. “People experience vaginal dryness because of the drop in estrogen associated with menopause.” This broad term can include vaginal dryness, burning and irritation, pain with sex, a lack of vaginal lubrication, urinary tract infections, urinary urgency and pain with urination.
“Studies show that up to 80 percent of women will experience one or several GSM symptoms, ranging from mild to major, over the course of their lifetime,” says Dr. Jeanne Bouteau, an OB/GYN at the Centre hospitalier de l’Université de Montréal and assistant professor at the Université de Montréal School
of Medicine. Despite this staggering statistic, few women speak to a loved one or even a medical professional about what they’re going through, usually because they believe it’s just a normal part of aging or they feel they’re not having enough sex to warrant treatment or they’re simply not comfortable bringing it up—even despite bothersome symptoms. “We can treat symptoms quite safely and long- term for patients of all ages,” says Bouteau, who specializes in menopause health. “Don’t wait to reach out to a health professional, since vaginal dryness and its many symptoms won’t disappear on their own like other menopause-related problems. Symptoms usually get worse, unlike hot flashes, which tend to get better over time.”
“Symptoms usually get worse, unlike hot flashes, which tend to get better over time.”
Shirreff agrees. “Speak to your doctor,” she says. “Sometimes other worrisome conditions need to be ruled out. It is important that people get reliable, evidence-based information about their health. Resources such as the ones created by our Gynaecology Quality Improvement Collaboration [Gynqi.com] are Canadian and offer information on many areas of women’s health.”
Once less lovingly referred to as “vulvovaginal atrophy,” GSM can be identified by several symptoms, which patients may experience when approaching, during and after menopause. “Itching, discomfort, tingling, burning, excessive discharge (with or without odour), pain during sex, microlesions on the vulva or in the vagina, frequent urinary tract or vaginal infections and an urgent or frequent need to urinate,” says Dr. Rachel Bruneau, an expert in women’s health at MAclinique Lebourgneuf in Quebec City, citing the main symptoms.
These telltale signs don’t always happen all at once or with the same intensity. Even if you’re dealing with just one issue, it’s important to get in touch with a medical professional (either your family doctor, a gynecologist or a specialized nurse practitioner) right away. “Please don’t be afraid to discuss this with a professional, even if you’re only experiencing mild symptoms,” says Bruneau. “There are many simple and accessible treatments that can have a significant impact on quality of life for women, who all too often suffer in silence. I like to joke with my patients that if men had similar issues affecting their penis, we’d be hearing about it all day long. So we shouldn’t hold back either!”
For women experiencing vaginal- dryness symptoms, some of the safest and most common methods for treating them include vaginal moisturizers (such as Replens, Gynalac and RepaGyn); local estrogens, like Premarin, Estragyn and Vagifem (which come in cream, pill, suppository or vaginal-ring form); prasterone (which is also known as DHEA and sold under the brand name Intrarosa), a steroid that’s absorbed by vaginal tissue; and ospemifene (which is sold under the brand name Osphena), the first selective estrogen- receptor modulator offered as an oral medication. Available only recently in Canada, ospemifene doesn’t contain hormones, but it does act like estrogen in certain target areas of the body. “It’s a new and promising option for people who don’t tolerate or want local treatments,” says Dr. Cleve Ziegler, an OB/GYN at the Jewish General Hospital in Montreal and an assistant professor of obstetrics and gynecology at McGill University.
And if you’re avoiding sex because of discomfort or pain, clinical sex therapist and psychotherapist Véronique Jodoin suggests meeting with an expert one on one or alongside your partner. “Less sex can cause friction in a relationship,” says Jodoin. “Your partner may not understand why and may feel like it’s their fault. That’s why I always recommend unpacking these issues with a therapist.”
Although GSM and everything that comes with it might be uncomfortable and hard to deal with, rest assured that so many women go through this and there are solutions out there to help.
*Name has been changed.
Newsletter
Join our mailing list for the latest and biggest in fashion trends, beauty, culture and celebrity.
Read Next

Fashion
Tennis Champions Roger Federer and Rafael Nadal Climb a Mountain With Louis Vuitton
An Odyssey of rivals turned friends.
by : Allie Turner- May 18th, 2024

Culture
Two ‘Bridgerton’ Cast Members Are Dating IRL
The Ton is a-twitter with rumours.
by : Rebecca Mitchell- May 17th, 2024
Culture
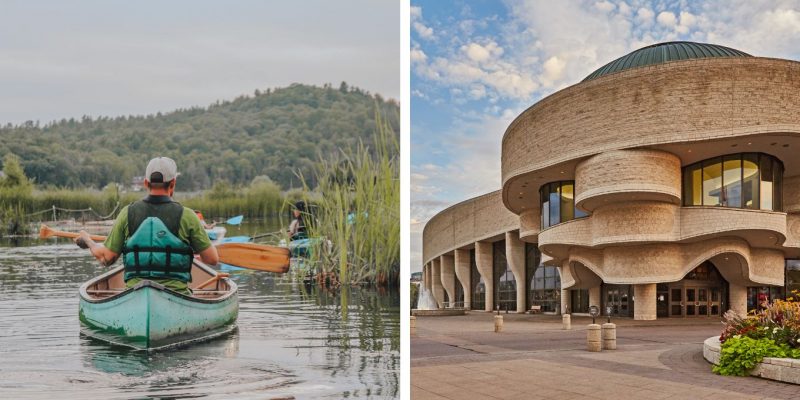
This Quebec Weekend Itinerary Takes the Scenic Route
The Outaouais has it all.
by : ELLE Canada- May 13th, 2024




